Knudsen, L., Lopez-Rodriguez, E., Berndt, L., Steffen, L., Ruppert, C., Bates, J.H.T., Ochs, M., Smith, B.J.: Am J Resp Cell Mol. 2018;59(6):757-69.
To access the full article, click here:

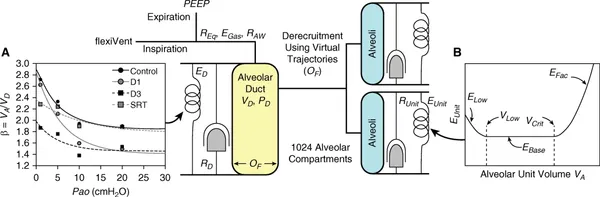
Lung injury results in intratidal alveolar recruitment and derecruitment and alveolar collapse, creating stress concentrators that increase strain and aggravate injury. In this work, we sought to describe alveolar micromechanics during mechanical ventilation in bleomycin-induced lung injury and surfactant replacement therapy. Structure and function were assessed in rats 1 day and 3 days after intratracheal bleomycin instillation and after surfactant replacement therapy. Pulmonary system mechanics were measured during ventilation with positive end-expiratory pressures (PEEPs) between 1 and 10 cm H2O, followed by perfusion fixation at end-expiratory pressure at airway opening (Pao) values of 1, 5, 10, and 20 cm H2O for quantitative analyses of lung structure. Lung structure and function were used to parameterize a physiologically based, multicompartment computational model of alveolar micromechanics. In healthy controls, the numbers of open alveoli remained stable in a range of Pao = 1–20 cm H2O, whereas bleomycin-challenged lungs demonstrated progressive alveolar derecruitment with Pao < 10 cm H2O. At Day 3, ∼40% of the alveoli remained closed at high Pao, and alveolar size heterogeneity increased. Simulations of injured lungs predicted that alveolar recruitment pressures were much greater than the derecruitment pressures, so that minimal intratidal recruitment and derecruitment occurred during mechanical ventilation with a tidal volume of 10 ml/kg body weight over a range of PEEPs. However, the simulations also predicted a dramatic increase in alveolar strain with injury that we attribute to alveolar interdependence. These findings suggest that in progressive lung injury, alveolar collapse with increased distension of patent (open) alveoli dominates alveolar micromechanics. PEEP and surfactant substitution reduce alveolar collapse and dynamic strain but increase static strain.