Krischer, J.M., Albert, K., Pfaffenroth, A., Lopez-Rodriguez, E., Ruppert, C., Smith, B.J., Knudsen, L.: Histochem Cell Biol. 2021;155(2):183-202.
To access the full article, click here:

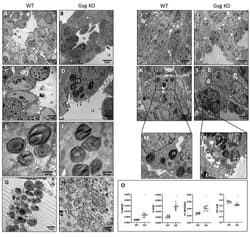
Mechanical ventilation triggers the manifestation of lung injury and pre-injured lungs are more susceptible. Ventilation-induced abnormalities of alveolar surfactant are involved in injury progression. The effects of mechanical ventilation on the surfactant system might be different in healthy compared to pre-injured lungs. In the present study, we investigated the effects of different positive end-expiratory pressure (PEEP) ventilations on the structure of the blood–gas barrier, the ultrastructure of alveolar epithelial type II (AE2) cells and the intracellular surfactant pool (= lamellar bodies, LB). Rats were randomized into bleomycin-pre-injured or healthy control groups. One day later, rats were either not ventilated, or ventilated with PEEP = 1 or 5 cmH2O and a tidal volume of 10 ml/kg bodyweight for 3 h. Left lungs were subjected to design-based stereology, right lungs to measurements of surfactant proteins (SP−) B and C expression. In pre-injured lungs without ventilation, the expression of SP-C was reduced by bleomycin; while, there were fewer and larger LB compared to healthy lungs. PEEP = 1 cmH2O ventilation of bleomycin-injured lungs was linked with the thickest blood–gas barrier due to increased septal interstitial volumes. In healthy lungs, increasing PEEP levels reduced mean AE2 cell size and volume of LB per AE2 cell; while in pre-injured lungs, volumes of AE2 cells and LB per cell remained stable across PEEPs. Instead, in pre-injured lungs, increasing PEEP levels increased the number and decreased the mean size of LB. In conclusion, mechanical ventilation-induced alterations in LB ultrastructure differ between healthy and pre-injured lungs. PEEP = 1 cmH2O but not PEEP = 5 cmH2O ventilation aggravated septal interstitial abnormalities after bleomycin challenge.