Beike, L., Wrede, C., Hegermann, J., Lopez-Rodriguez, E., Kloth, C., Gauldie, J., Kolb, M., Maus, U.A., Ochs, M., Knudsen, L.: Lab Invest. 2019;99(6):830-52.
To access the full article, click here:

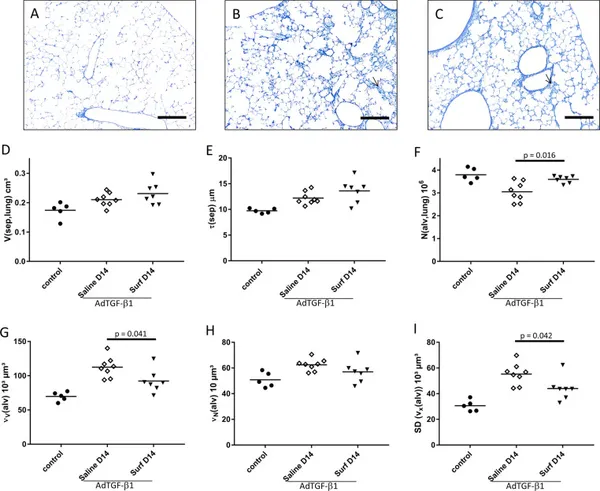
In human idiopathic pulmonary fibrosis (IPF), collapse of distal airspaces occurs in areas of the lung not (yet) remodeled. Mice lungs overexpressing transforming growth factor-β1 (TGF-β1) recapitulate this abnormality: surfactant dysfunction results in alveolar collapse preceding fibrosis and loss of alveolar epithelial type II (AE2) cells' apical membrane surface area. Here we examined whether surfactant dysfunction-related alveolar collapse due to TGF-β1 overexpression is linked to septal wall remodeling and AE2 cell abnormalities. Three and 6 days after gene transfer of TGF-β1, mice received either intratracheal surfactant (Surf-groups: Curosurf®, 100 mg/kg bodyweight) or 0.9% NaCl (Saline-groups). On days 7 (D7) and 14 (D14), lung mechanics were assessed followed by design-based stereology at light and electron microscopic level to quantify structures. Compared with Saline, Surf showed significantly improved tissue elastance, increased numbers of open alveoli, as well as reduced alveolar size heterogeneity on D7. Deterioration in lung mechanics was highly correlated to the loss of open alveoli. On D14, lung mechanics, number of open alveoli, and alveolar size heterogeneity remained significantly improved in the Surf-group. Volumes of extracellular matrix and collagen fibrils in septal walls were significantly reduced, whereas the apical membrane surface area of AE2 cells was increased in Surf compared with Saline. In remodeled tissue with collapsed alveoli, three-dimensional reconstruction of AE2 cells based on scanning electron microscopy array tomography revealed that AE2 cells were trapped without contact to airspaces in the TGF-β1 mouse model. Similar observations were made in human IPF. Based on correlation analyses, the number of open alveoli and of alveolar size heterogeneity were highly linked with the loss of apical membrane surface area of AE2 cells and deposition of collagen fibrils in septal walls on D14. In conclusion, surfactant replacement therapy stabilizes alveoli and prevents extracellular matrix deposition in septal walls in the TGF-β1 model.